Project Overview:
This project was completed as part of a medical device design class at the University of Cincinnati. I was on a team of three, with all members contributing to the design, research, and documentation. We were presented with the clinical problem by a medical student, and had roughly one-and-a-half months to conduct background research, ideate potential solutions, select a design, model the design in CAD, and complete a design history file. This project taught me how to down-select from competing design concepts, how to translate user needs into design requirements, and how to effectively utilize team members' skills to produce the best results. The highlights of this project are shown below. The complete Design History File can be found here.
This project was completed as part of a medical device design class at the University of Cincinnati. I was on a team of three, with all members contributing to the design, research, and documentation. We were presented with the clinical problem by a medical student, and had roughly one-and-a-half months to conduct background research, ideate potential solutions, select a design, model the design in CAD, and complete a design history file. This project taught me how to down-select from competing design concepts, how to translate user needs into design requirements, and how to effectively utilize team members' skills to produce the best results. The highlights of this project are shown below. The complete Design History File can be found here.
Background Information:
Airway stenosis is a narrowing of the airway that prevents the passage of air into the lungs. Airway stenosis can occur for several reasons including congenital conditions, cancer, external injury, or some autoimmune disorders. The symptoms of airway stenosis include coughing, wheezing, labored breathing, and cyanosis (a bluish color of the skin or mucus membranes) (Riley Children’s Health). Airway stenosis is a rare disease, it only occurs in one out of four hundred thousand people. However, in pediatric patients, subglottic airway stenosis can be fatal since a pediatric subglottic diameter is about four millimeters (Mayo Clinic, 2019).
Airway stenosis is diagnosed by x-ray, computed tomography (CT) scans, laryngoscopy, or bronchoscopy. Imaging is a useful tool for diagnosis but is not accurate enough to determine the surgical tools needed. Imaging is done to diagnose the patient and determine the relative size and shape of the stenosis and then a laryngeal sizing device is used immediately before surgery to check the size of the airway and then also after surgery to check the size of the intervention. Though this method is more invasive and can potentially cause further inflammation, the diameter of the airway is important to know for treatment. The airway size can change from the time of imaging to surgery. The airway size will also affect the amount of anesthesia needed (A. Jain, personal communication, March 24th, 2022). Airway stenosis is treated with surgery either by placing a stent to keep the airway open or by cutting away the obstruction (Cotton & Smith, 2018). The airway size is important to know for surgical planning because it drives which operating tools are chosen (A. Jain, personal communication, March 24th, 2022).
Design Objective:
The desired device will be used to provide an accurate measurement of the pediatric patient’s airway stenosis to the surgical team. This information is vital in the planning of the surgery and the use of tools during the procedure. The diameter of a pediatric trachea is usually around 4 millimeters (about 0.16 in). This small diameter, with a stenosis making this even smaller, requires a device that is small enough to fit in the airway without damaging the surrounding tissue.
User Needs:
UN 1
Surgeons must measure the diameter of airway stenosis in pediatric patients prior to surgery.
Users need a way to safely measure the diameter of airway stenosis.
UN 2
A handheld device is used to measure the pediatric airway prior to surgery.
Users need a comfortable, handheld device that fits a range of surgeons’ hand sizes.
UN 3
A simple device is desired to make the measurement process quick and efficient.
User needs a device that is simple and quickly measures the airway stenosis to streamline the procedure preparation.
UN 4
The device needs to prevent further damage and inflammation to the patient’s trachea during the measurement process.
Users need a device that can be used in conjunction with a camera to enable a visual on the device’s location in the trachea to prevent further tissue damage.
UN 5
Pediatric subglottic diameters are around 4mm (about 0.16 in) in diameter, and airway stenosis decreases this diameter.
Users need a small device that can be used to measure a range of stenosis severity grades in pediatric patients.
UN 6
Accurate measurements of airway stenosis determine the path of the surgical procedures and tools used.
Users need a device that is calibrated to give accurate measurements of the airway stenosis severity.
UN 7
Users do not have time to read a small ruler accurately through a camera in the patient’s airway.
Users need a visual indication on the device to display the measurement of the airway stenosis once measured by the device.
Initial Concepts:
Airway stenosis is a narrowing of the airway that prevents the passage of air into the lungs. Airway stenosis can occur for several reasons including congenital conditions, cancer, external injury, or some autoimmune disorders. The symptoms of airway stenosis include coughing, wheezing, labored breathing, and cyanosis (a bluish color of the skin or mucus membranes) (Riley Children’s Health). Airway stenosis is a rare disease, it only occurs in one out of four hundred thousand people. However, in pediatric patients, subglottic airway stenosis can be fatal since a pediatric subglottic diameter is about four millimeters (Mayo Clinic, 2019).
Airway stenosis is diagnosed by x-ray, computed tomography (CT) scans, laryngoscopy, or bronchoscopy. Imaging is a useful tool for diagnosis but is not accurate enough to determine the surgical tools needed. Imaging is done to diagnose the patient and determine the relative size and shape of the stenosis and then a laryngeal sizing device is used immediately before surgery to check the size of the airway and then also after surgery to check the size of the intervention. Though this method is more invasive and can potentially cause further inflammation, the diameter of the airway is important to know for treatment. The airway size can change from the time of imaging to surgery. The airway size will also affect the amount of anesthesia needed (A. Jain, personal communication, March 24th, 2022). Airway stenosis is treated with surgery either by placing a stent to keep the airway open or by cutting away the obstruction (Cotton & Smith, 2018). The airway size is important to know for surgical planning because it drives which operating tools are chosen (A. Jain, personal communication, March 24th, 2022).
Design Objective:
The desired device will be used to provide an accurate measurement of the pediatric patient’s airway stenosis to the surgical team. This information is vital in the planning of the surgery and the use of tools during the procedure. The diameter of a pediatric trachea is usually around 4 millimeters (about 0.16 in). This small diameter, with a stenosis making this even smaller, requires a device that is small enough to fit in the airway without damaging the surrounding tissue.
User Needs:
UN 1
Surgeons must measure the diameter of airway stenosis in pediatric patients prior to surgery.
Users need a way to safely measure the diameter of airway stenosis.
UN 2
A handheld device is used to measure the pediatric airway prior to surgery.
Users need a comfortable, handheld device that fits a range of surgeons’ hand sizes.
UN 3
A simple device is desired to make the measurement process quick and efficient.
User needs a device that is simple and quickly measures the airway stenosis to streamline the procedure preparation.
UN 4
The device needs to prevent further damage and inflammation to the patient’s trachea during the measurement process.
Users need a device that can be used in conjunction with a camera to enable a visual on the device’s location in the trachea to prevent further tissue damage.
UN 5
Pediatric subglottic diameters are around 4mm (about 0.16 in) in diameter, and airway stenosis decreases this diameter.
Users need a small device that can be used to measure a range of stenosis severity grades in pediatric patients.
UN 6
Accurate measurements of airway stenosis determine the path of the surgical procedures and tools used.
Users need a device that is calibrated to give accurate measurements of the airway stenosis severity.
UN 7
Users do not have time to read a small ruler accurately through a camera in the patient’s airway.
Users need a visual indication on the device to display the measurement of the airway stenosis once measured by the device.
Initial Concepts:
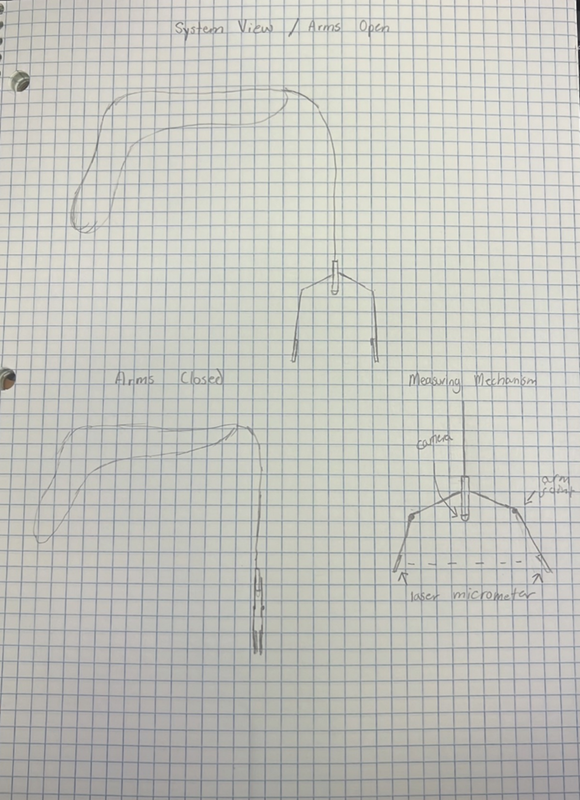
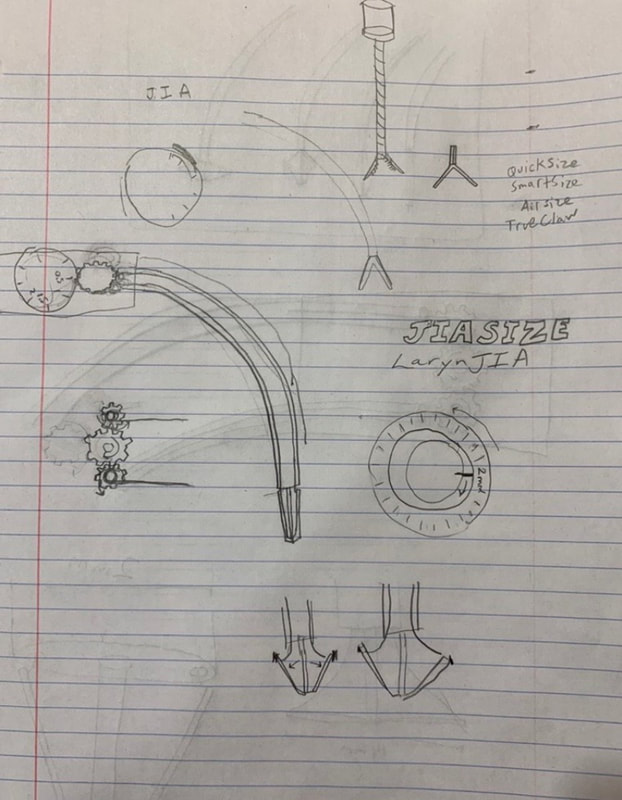
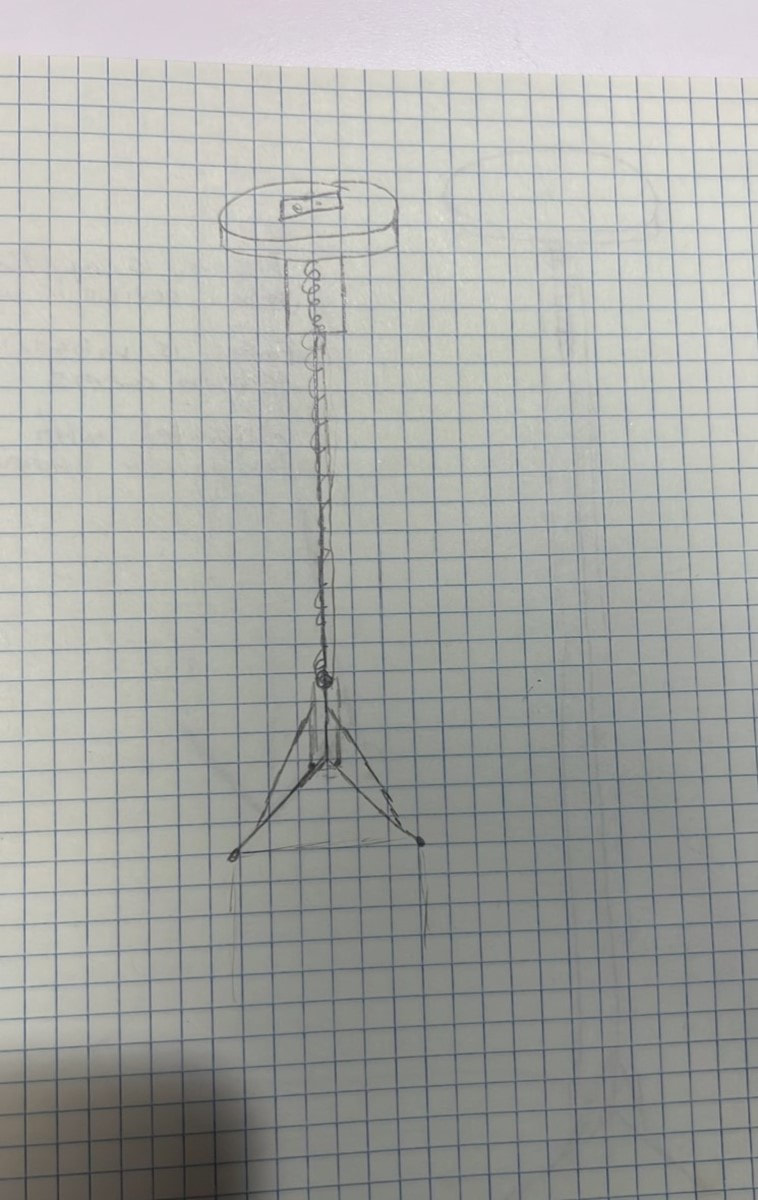
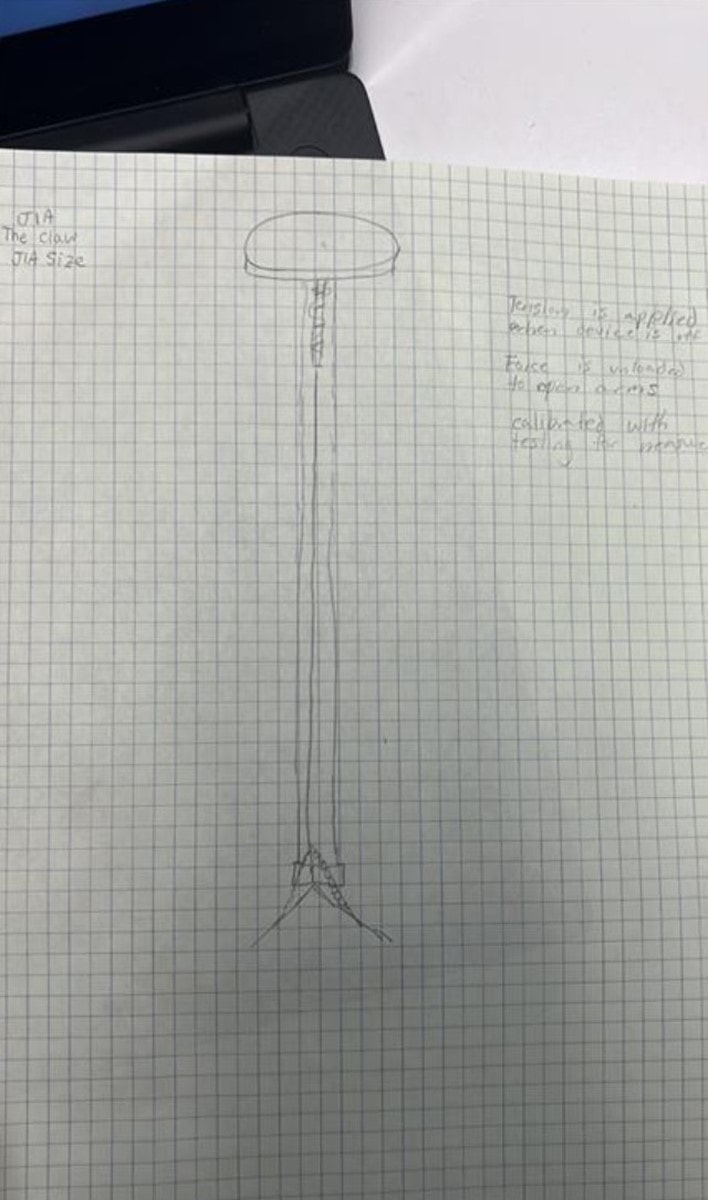
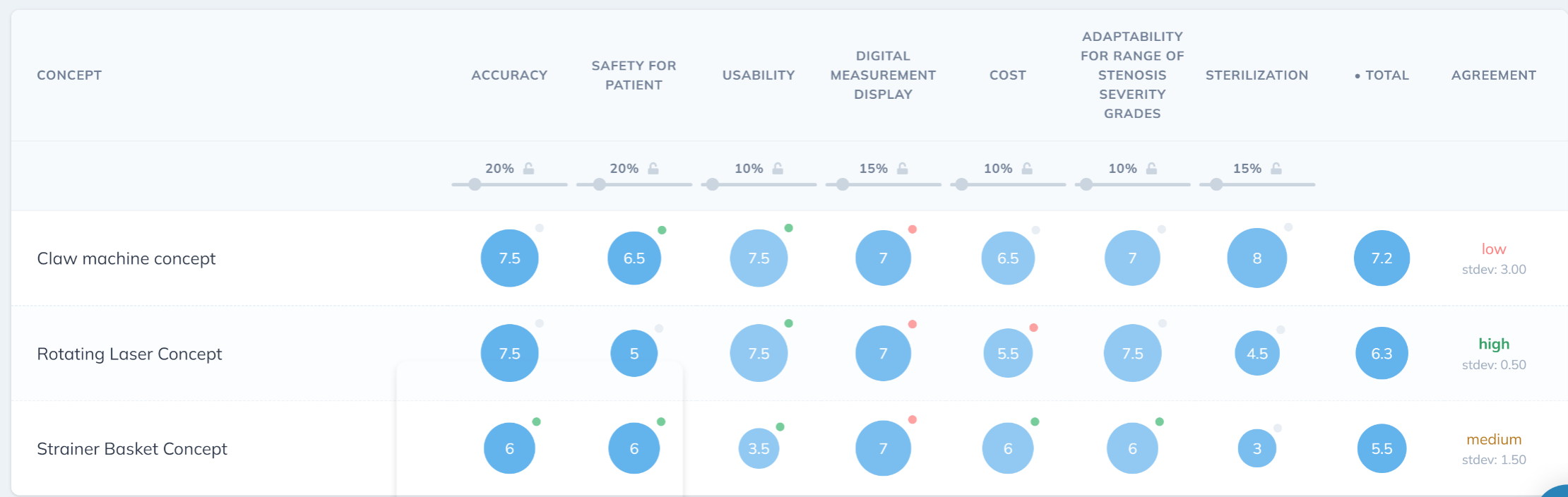
- Claw Machine Concept
- When the device is “off” the hands of the device are closed so that the user can insert the device without contact with the walls of the trachea. The user will turn a dial at the top of the device causing the hands of the device to open. The distance between the hands will measure the size of stenosis.
- Advantages: Collapsible so the device can be safely inserted and removed
- Disadvantages: Small intricate parts
- Overlapping Strainer Concept
- The overlapping pieces of material open similarly to a strainer basket. The diameter of the circle made by the end of the device will measure the stenosis.
- Advantages: Collapsible
- Disadvantages: Intricate parts and spaces that could store bacteria
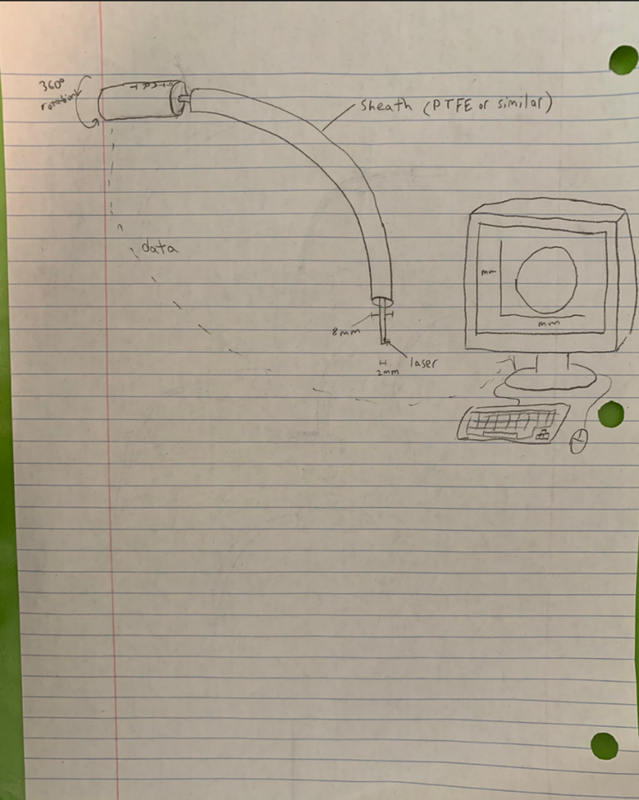
- Rotating Laser Concept
- A Plastic tube will be inserted into the throat. A wire with a rotating laser will be inserted through the tube. The laser will rotate 360 degrees and measure the throat by measuring the time that it takes for the light to bounce back.
- Advantages: Reusable, Thin (Safe for insertion and removal)
- Disadvantages: Lasers make for difficult clinical trials, could cause damage (A. Jain, personal communication, March 24th, 2022).
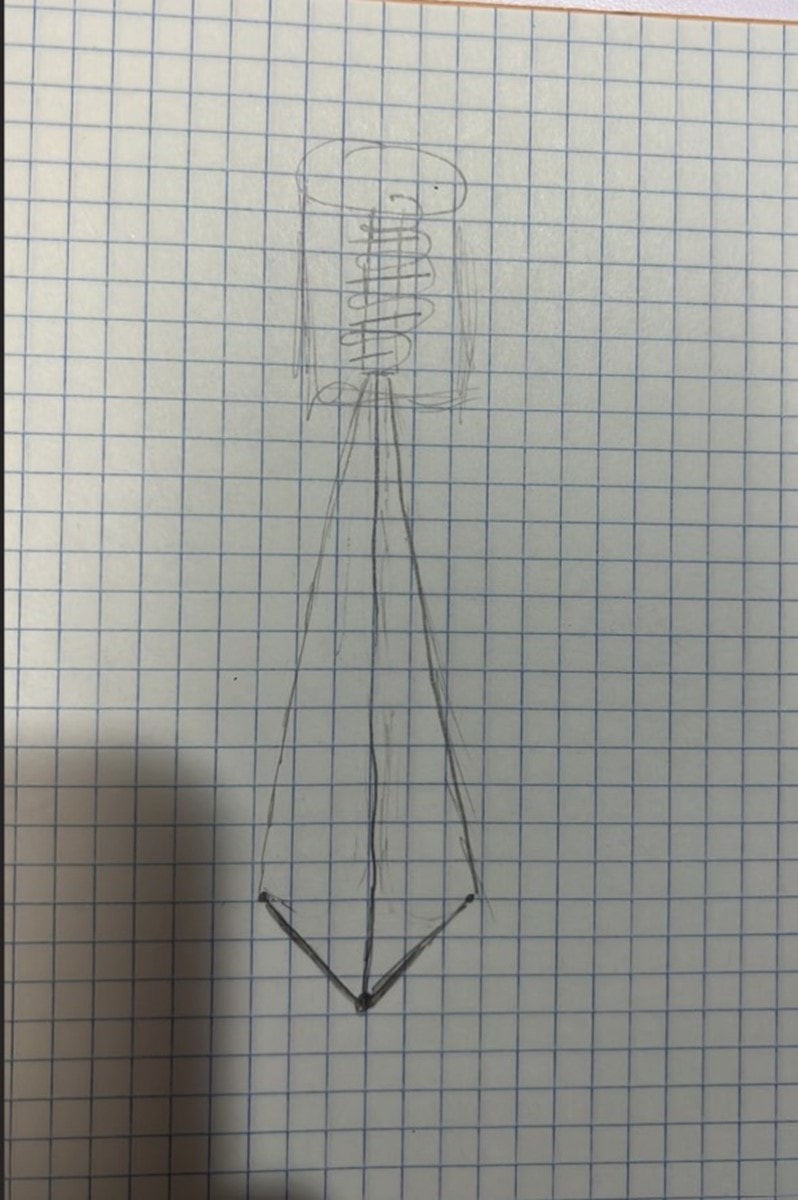
- Spring with internal tension wire
- Description: Spring capsule with wire running through the interior wire attached to the dial and to the arms of the device. Turning the dial pulls the arms up. The distance between the hands of the device measures the diameter of the airway.
- Advantage: Cheap materials
- Disadvantage: Spring negatively impacts function by adding additional tension to the internal wire
- Plastic Tube with internal tension wire
- Description: Flexible plastic tube with wire in the interior, wire attached to the dial. When the dial is turned the wire coils around it. Wire connected to the arms of the device
- Advantages: Cheap materials
- Disadvantages: Tube negatively impacts function by adding additional tension to the internal wire
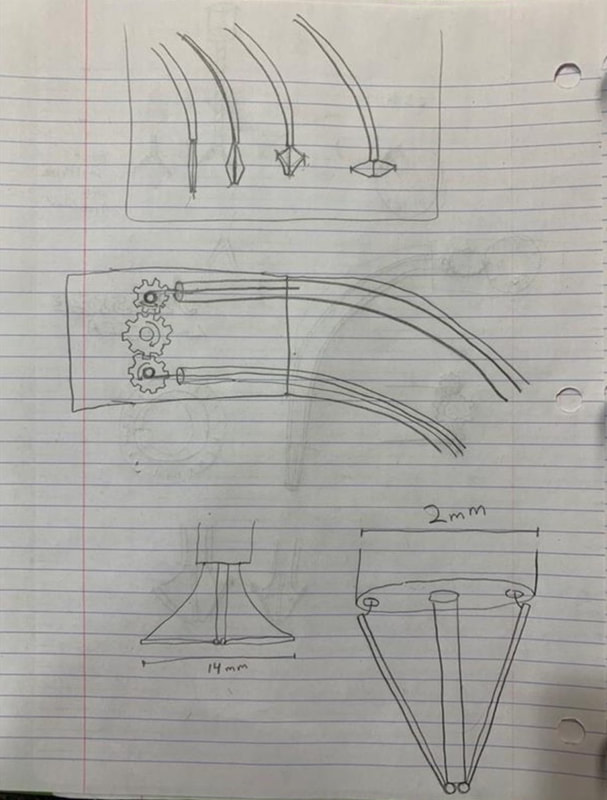
- Interlocking Gears
- Description: Turning gears opens arms, wire coils as gear turns
- Advantages: Mechanical strength
- Disadvantages: expensive
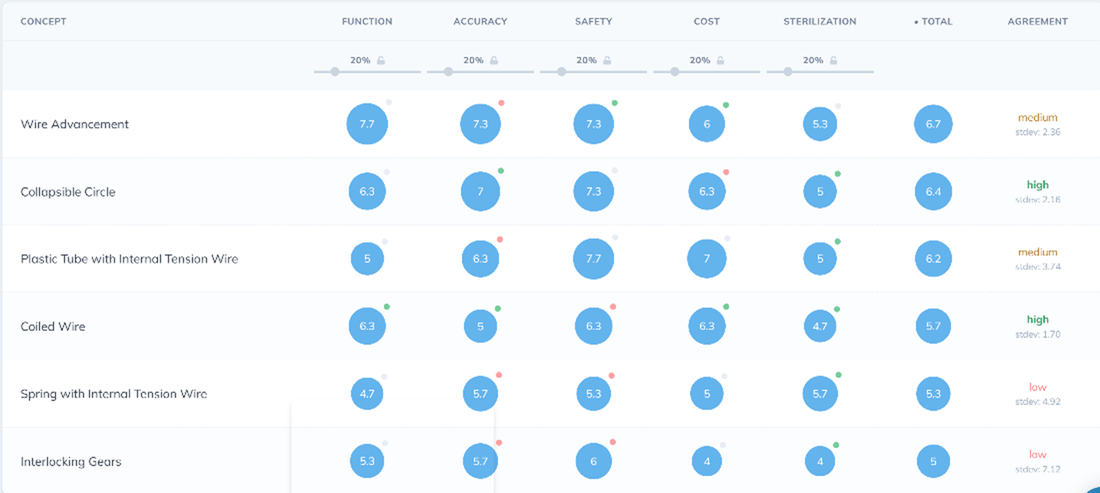
- Wire advancement
- Description: Gears turn to release wires. Wires attach to the tips of the arms and release the arms when the wires increase in length.
- Advantages: functional, gears are mechanically strong
- Disadvantages: sterilization is complicated, could create a prong that can get caught in tissue
- Collapsible Circle
- Description: Flexible, collapsible sphere compresses into flat disk, largest cross section diameter measures airway size
- Advantages: No sharp edges, safest concept
- Disadvantages: Complicated Manufacturing
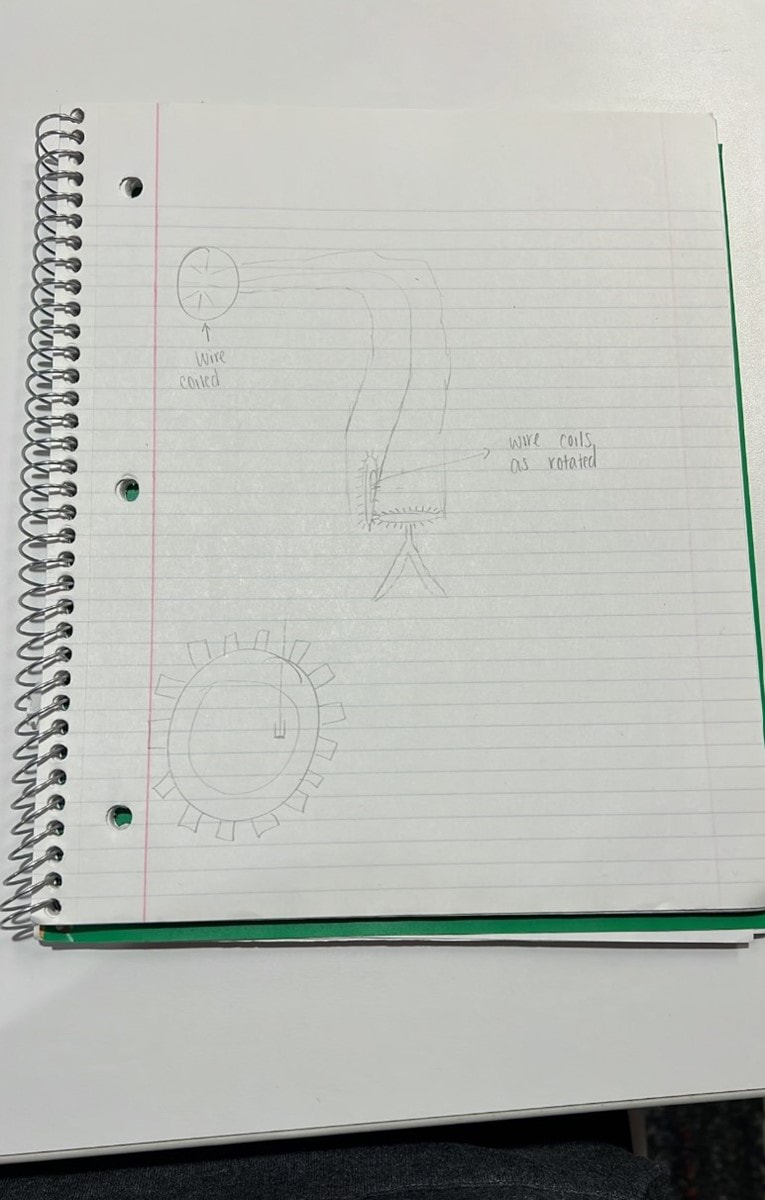
- Coiled Wire
- Description: Two wires attached to dial. Central flexible wire for mechanical strength. Turning dial releases wires opening the arms. Distance between tips of arms measures diameter of airway.
- Advantages: Simple materials, cost effective
- Disadvantages: Coil of wire is susceptible to wear, and the two wires can tangle.
Selected Concept:
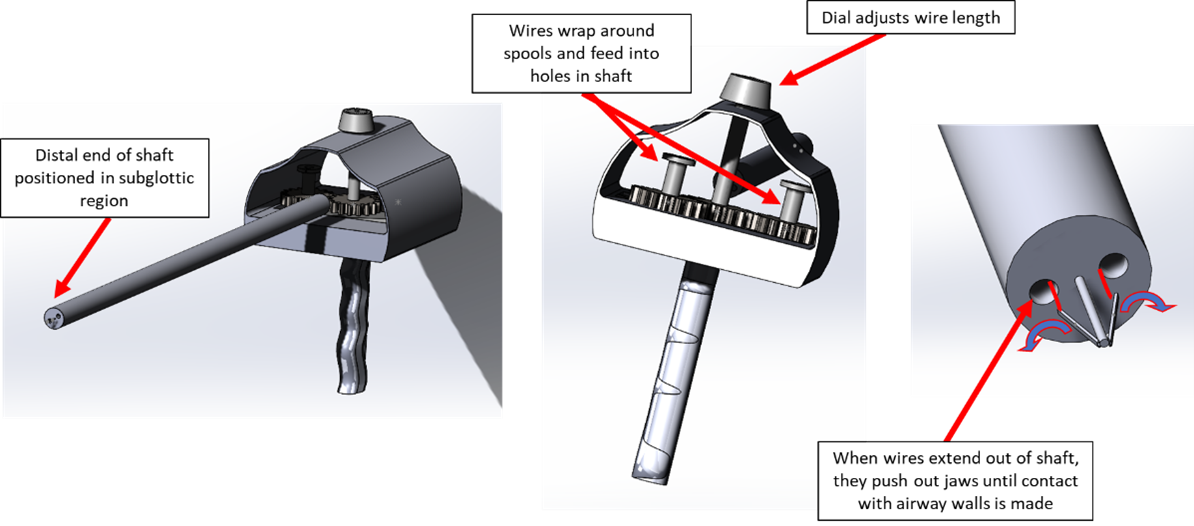
The selected concept consists of a handle with a circular dial that is connected to a flexible shaft that is inserted into the airway. At the distal end of the shaft are two jaws that open and close when the dial on the handle is rotated. The dial is connected to gears that, when turned, feed out two wires from an internal spool. The distal ends of the wires are connected to the proximal ends of the jaws, so that as the wires are fed out from the spool, the jaws are pushed outward. The dial shall be rotated until the jaws expand to the point at which they make contact with the walls of the airway.
The selected concept consists of a handle with a circular dial that is connected to a flexible shaft that is inserted into the airway. At the distal end of the shaft are two jaws that open and close when the dial on the handle is rotated. The dial is connected to gears that, when turned, feed out two wires from an internal spool. The distal ends of the wires are connected to the proximal ends of the jaws, so that as the wires are fed out from the spool, the jaws are pushed outward. The dial shall be rotated until the jaws expand to the point at which they make contact with the walls of the airway.